Le compagnon qui veille sur la santé des femmes et bébés du monde

Efelya a été pensé pour :
Vous accompagner médicalement et vous informer
Avant, pendant et après votre grossesse, grâce à des centaines d'articles, de vidéos, de podcasts réalisés par des professionnels de la santé.
Vous rassurer, vous conseiller
Grâce aux échanges personnalisés avec notre équipe de praticiens via notre messagerie sécurisée.
Vous dépister
Dépister les grossesses à risque par l'élaboration d'un profil de risque personnalisé autour des 6 pathologies de grossesses les plus communes : diabète gestationnel, hypertension, prééclampsie, risque d'accouchement prématuré, retard de croissance intra-utérin et risque hémorragique.
Télécharger Efelya
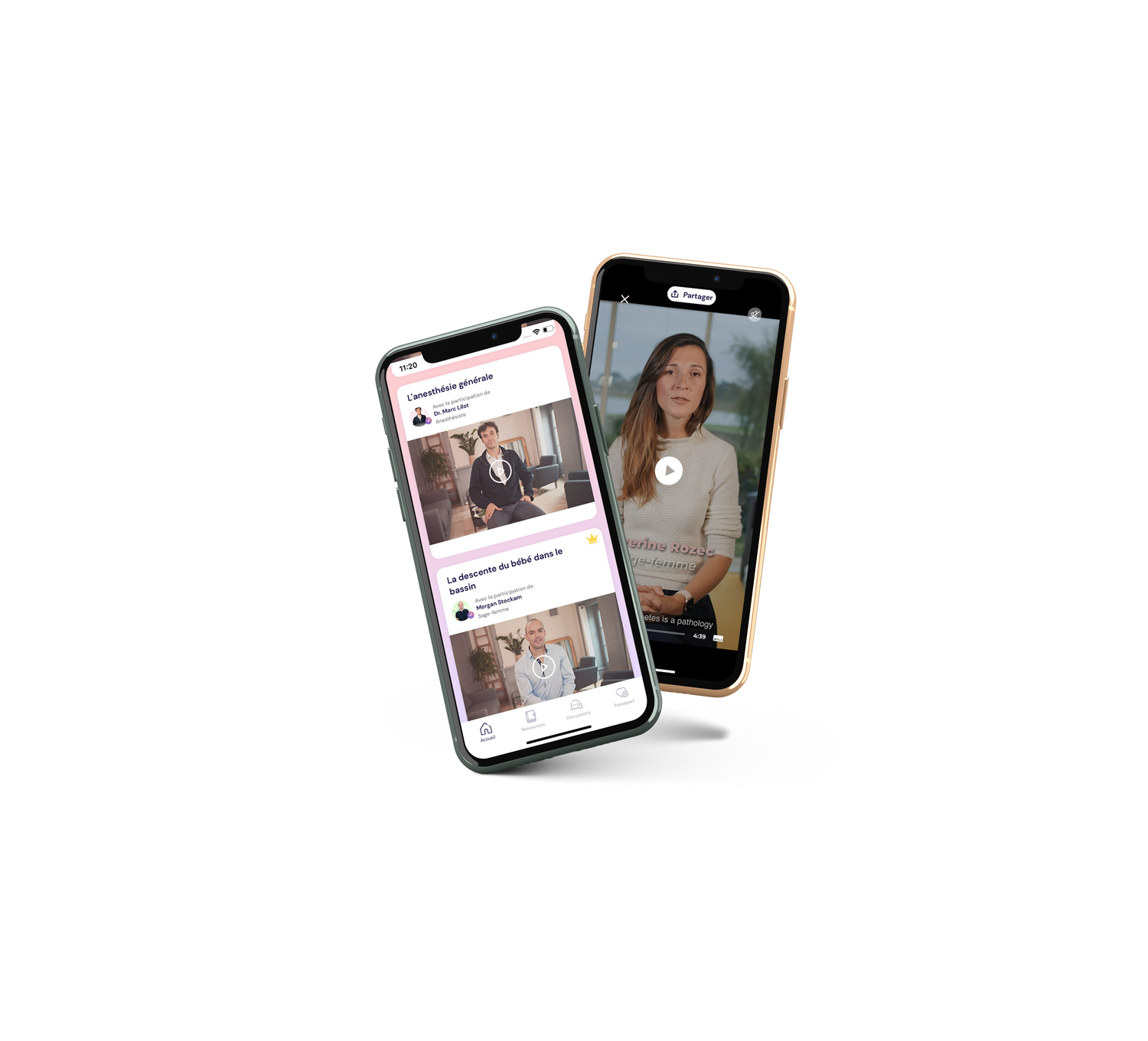
Nos experts
Découvrez notre équipe d'experts médicaux pluridisciplinaires,
qui vous guidera tout au long de votre grossesse !
Sages-femmes, gynécologues-obstétriciens, pharmaciens, anesthésiste,biologistes,médecins addictologues, dentistes, ostéopathes, psychologues, kinésithérapeutes, sophrologues, diététiciennes.